Note: I am republishing this to my email subscribers because none of the links worked the first time around. I’ve fixed everything now – so sorry for the error – must have been healthcare fatigue!
**************************************************************************
I’ve noticed that a lot of people in healthcare seem unusually tired and even, if I dare say so, somewhat cranky. This includes me. I’ve decided we’re all suffering from healthcare fatigue – fatigue from dealing on a daily basis with so much change, uncertainty, and financial stress. Here’s my top ten list of healthcare management stressors accompanied by posts I’ve written that discuss the topic or suggest resources for the challenge.
10. Red Flags Rules – on again, off again, patients don’t want to have their pictures taken or let you copy their driver’s licenses.
- Red Flags Rules (RFR) Delayed for the Fifth Time ”“ This Time Until December 31, 2010
- Red Flags Rule and Identity Theft Prevention: You Don’t Have To, But You Should!

Image by purpleslog via Flickr
9. HIPAA – don’t be fooled, HIPAA is not something we handled years ago and it’s taken care of; there are new requirements and penalties associated with HIPAA breaches. HIPAA is a biggie and something that now infiltrates almost every facet of healthcare.
8. Employment Uncertainty – both for you and your staff – the aftermath of layoffs can be even more demoralizing to those who didn’t lose their jobs. Also, many healthcare entities are still freezing raises. If I hear one more time “we’ll just have to do more with less” I might just scream.
- My Take on “10 Ways to Keep Employees Happy” in Medical Practices
- Dear Mary Pat: Should Staff Be Allowed to Use The Internet on Their Smart Phones at Work?

Image by jcoterhals via Flickr
7. Unrealistic Workloads – directly related to #9, most staff and managers have much more work to do than they did just two years ago. Couple that with the ability for managers to be available and work by computer, phone, text message, email or Skype 24/7 and you have fatique that you understand only when you truly, truly stop and wind down for more than three days at a time.
6. Hospitals Buying Practices – this could be a good thing or a bad thing, but as you and I know, change is completely unnerving to most people. Hospitals have very different cultures than private practices and trying to marry the two takes skill, patience and excellent leadership.
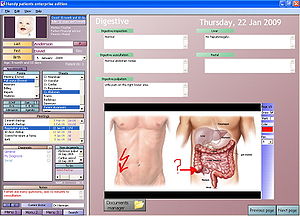
Image via Wikipedia
5. Stimulus Money for Using EMRs – it’s a big decision and many practices are very nervous about purchasing an EMR. Many think that meaningful use components are unrealistic and even more are fearful of the inevitable productivity drop when the EMR is implemented and for months afterwards.
- ARRA Eligible Providers: Who Is Eligible to Receive Stimulus Money and How Much is Available Per Provider?
- FAQ on HITECH, Meaningful Use, Eligible Providers, and the Stimulus Money
- Ten Reasons Why (Some) Physicians Aren’t Rushing to Adopt EMRs
- Electronic Medical Record Guru Rosemarie Nelson Reveals Best EMR Product on the Market Today
4. Unhappy Patients – lots of patients are also trying to do more with less (argghhh!) and are avoiding coming to the doctor whenever possible. The front desk staff and the phone staff in particular are getting a lot more heat when they inform patients they’ll have to make an appointment.
- 50 Customer Service Ideas to Treat Your Patients to Friendly, Easy and Unexpected Service
- How To Be A Billing Advocate for Your Patients
- How to Apologize to a Patient
- A Memo to the Staff: The Preciousness of Patients
3. PECOS – be glad if you don’t know what PECOS stands for, or be very, very afraid.
- Providers Without a PECOS Record Will Receive a Letter From Their Medicare Administrative Contractor (MAC)
- My Notes from the CMS Open Door Forum on May 19, 2010: PECOS, DMEPOS and Blue Ink on Paper Forms
- Is Your Practice Ready for the 60-Day PECOS Countdown?
2. Medicare Reimbursement – this year has been as exhausting as watching a single point of ping pong played for hours – there will be cuts, there won’t be cuts, there will be cuts, there won’t be cuts. Gird your loins as the November 30 deadline looms for the next potential cuts.

Image by longhorndave via Flickr
- Deja Vu All Over Again: The Medicare Fee Cut is Pushed Back to November 30, 2010
- Attention Medical Practice Staff: Medicare Changes the Rules for Credentialing and Retro-Billing
- 91 Physician Organizations Sign Statement Naming Congress in “Mismanagement of the Medicare Program” and Imploring it to “Honor its Obligation”
1. The Bottom Line – we have RAC audits, more pre-certification and pre-authorization and pre-notification requirements, more denials, high deductible plans, formularies and 50 other things that are making it difficult to know which hoop to jump through to get paid. Expenses continue to go up, reimbursement continues to go down, and the healthcare world spins faster and harder, making us all wonder when it will, or if it ever will slow down.


