e-RX: Medicare e-prescribing hardship exemptions under review (jump to story)
EFT: suppliers and providers who are not currently receiving Medicare EFT payments are required to submit the CMS-588 EFT form (jump to story)
SNFs: Allowing Physician Assistants to Perform Skilled Nursing Facility (SNF) Level of Care Certifications and Recertifications (jump to story)
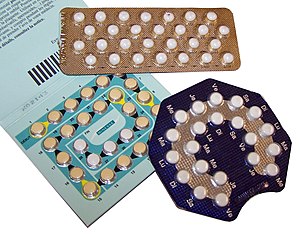
ACA: the final rule on preventive health services will ensure that women with health insurance coverage will have access to the full range of the Institute of Medicine’s recommended preventive services, including all FDA -approved forms of contraception. (jump to story)
EHR Incentive Program: what can still be completed in 2012 in order to receive an incentive payment for CY2011 (jump to story)
5010: National Provider Call: Medicare FFS Implementation of HIPAA Version 5010 and D.0 Transactions (jump to story)
Claims Crossovers: Greater instances of Medicare correspondence letters that make reference to error N22226 as the basis for patient claims not crossing over(jump to story)
ICD-10: What’s Your Plan, Man?(jump to story)
MLN: Medicare Learning Network Announcements, Updates and Revisions (jump to story)
——————————
Medicare e-prescribing hardship exemptions under review
Last fall, physicians had the opportunity to seek hardship exemptions and avoid penalties for failing to successfully participate in Medicare’s e-prescribing program. The Centers for Medicare & Medicaid Services (CMS) is reviewing each hardship exemption request on an individual basis and has not yet completed its analysis. Therefore, it is possible that some physicians will be subjected to a 1 percent Medicare payment penalty inappropriately until the backlog of exemption requests is reviewed. Ultimately, CMS will reprocess the claims.
Read information regarding remittance advice and information on the impact to physician reimbursement and patient copays. More information on the penalty program can be found here.
Find additional electronic prescribing information and resources on the AMA website.
The ACA (Affordable Care Act) Mandates Federal Payment to Providers and Suppliers Only by Electronic Means
Existing regulations at 42 CFR 424.510(e)(1)(2) require that at the time of enrollment, enrollment change request, or revalidation, providers and suppliers that expect to receive payment from Medicare for services provided must also agree to receive Medicare payments through electronic funds transfer (EFT). Section 1104 of the Affordable Care Act further expands Section 1862(a) of the Social Security Act by mandating federal payments to providers and suppliers only by electronic means. As part of CMS’s revalidation efforts, all suppliers and providers who are not currently receiving EFT payments are required to submit the CMS-588 EFT form with the Provider Enrollment Revalidation application, or at the time any change is being made to the provider enrollment record by the provider or supplier, or delegated official.
For more information about provider enrollment revalidation, review the Medicare Learning Network’s Special Edition Article #SE1126, titled “Further Details on the Revalidation of Provider Enrollment Information.”
——————————–
Allowing Physician Assistants to Perform Skilled Nursing Facility (SNF) Level of Care Certifications and Recertifications
http://www.cms.gov/
A Statement by U.S. Department of Health and Human Services Secretary Kathleen Sebelius
In August 2011, the Department of Health and Human Services issued an interim final rule that will require most health insurance plans to cover preventive services for women including recommended contraceptive services without charging a co-pay, co-insurance or a deductible. The rule allows certain non-profit religious employers that offer insurance to their employees the choice of whether or not to cover contraceptive services. Today the department is announcing that the final rule on preventive health services will ensure that women with health insurance coverage will have access to the full range of the Institute of Medicine’s recommended preventive services, including all FDA -approved forms of contraception. Women will not have to forego these services because of expensive co-pays or deductibles, or because an insurance plan doesn’t include contraceptive services. This rule is consistent with the laws in a majority of states which already require contraception coverage in health plans, and includes the exemption in the interim final rule allowing certain religious organizations not to provide contraception coverage. Beginning August 1, 2012, most new and renewed health plans will be required to cover these services without cost sharing for women across the country.
After evaluating comments, we have decided to add an additional element to the final rule. Nonprofit employers who, based on religious beliefs, do not currently provide contraceptive coverage in their insurance plan, will be provided an additional year, until August 1, 2013, to comply with the new law. Employers wishing to take advantage of the additional year must certify that they qualify for the delayed implementation. This additional year will allow these organizations more time and flexibility to adapt to this new rule. We intend to require employers that do not offer coverage of contraceptive services to provide notice to employees, which will also state that contraceptive services are available at sites such as community health centers, public clinics, and hospitals with income-based support. We will continue to work closely with religious groups during this transitional period to discuss their concerns.
Scientists have abundant evidence that birth control has significant health benefits for women and their families, it is documented to significantly reduce health costs, and is the most commonly taken drug in America by young and middle-aged women. This rule will provide women with greater access to contraception by requiring coverage and by prohibiting cost sharing.
This decision was made after very careful consideration, including the important concerns some have raised about religious liberty. I believe this proposal strikes the appropriate balance between respecting religious freedom and increasing access to important preventive services. The administration remains fully committed to its partnerships with faith-based organizations, which promote healthy communities and serve the common good. And this final rule will have no impact on the protections that existing conscience laws and regulations give to health care providers.
Receiving an EHR Incentive Program Payment for CY2011
As 2012 begins, CMS wants to remind eligible professionals (EPs) participating in the Medicare Electronic Health Record (EHR) Incentive Program of important deadlines approaching and what can still be completed in 2012 in order to receive an incentive payment for CY2011.
Important Medicare EHR Incentive Program Dates
On Saturday, December 31, 2011, the reporting year ended for EPs who participated in the Medicare EHR Incentive Program in 2011. What does this mean? For participating EPs, they must have completed their 90-day reporting period by the end of 2011.
However, EPs have until Wednesday, February 29, 2012 to actually register and attest to meeting meaningful use to receive an incentive payment for CY2011 through the Medicare & Medicaid EHR Incentive Program Registration and Attestation System.
Payment Threshold Information
Wednesday, February 29, 2012 is also the deadline for EPs to submit any pending Medicare Part B claims from CY2011, as CMS allows 60 days after Saturday, December 31, 2011 for all pending claims to be processed. This means that EPs have 60 days in 2012 to submit claims for allowed charges incurred in 2011.
Medicare EHR incentive payments to EPs are based on 75% of the Part B allowed charges for covered professional services furnished by the EP during the entire payment year. If the EP did not meet the $24,000 threshold in Part B allowed charges by the end of CY2011, CMS expects to issue an incentive payment for the EP in April 2012 for 75% of the EP’s Part B charges from 2011.
Note for Medicaid Participants: Medicaid incentives will be paid by the states, but the timing will vary according to state. Please contact your State Medicaid Agency for more details about payment.
Want more information about the EHR Incentive Programs? Visit the EHR Incentive Programs website for the latest news and updates on the EHR Incentive Programs.
——————————–
National Provider Call: Medicare FFS Implementation of HIPAA Version 5010 and D.0 Transactions – Register Now
Wednesday, January 25, 2012, 2-3:30pm ET
CMS will host a special National Provider Call regarding the Medicare FFS implementation of HIPAA Version 5010 and D.0 transaction standards.
Target Audience: Vendors, clearinghouses, and providers who need to make Medicare FFS-specific changes in compliance with HIPAA Version 5010 requirements.
Agenda (there will be no slide presentation for this call):
- HIPAA Version 5010 implementation update
- Question & answer session
If you would like to submit a question related to this topic in advance of, during, or following the call, please email your inquiry to the 5010 FFS Information resource mailbox at 5010FFSinfo@CMS.hhs.gov. Note that this resource box will only accept emails the day before, the day of, and the day after this call; your emailed questions will be answered as soon as possible, and may not be answered during the call.
Registration Information: In order to receive the call-in information, you must register for the call. Registration will close at 12pm on the day of the call or when available space has been filled; no exceptions will be made, so please register early. For more details, including instructions on registering for the call, please visit http://www.eventsvc.com/
Greater instances of Medicare correspondence letters that make reference to error N22226 as the basis for patient claims not crossing over
On Monday, December 5, 2011, CMS issued a Special Edition MLN Matters Article (SE1137) entitled “Additional Health Insurance Portability and Accountability Act (HIPAA) 837 5010 Transitional Changes and Further Modifications to the Coordination of Benefits Agreement (COBA) National Crossover Process.” CMS issued this guidance for the benefit of physicians/practitioners, providers, and suppliers to help them understand why they were seeing greater instances of Medicare correspondence letters that made reference to error N22226 as the basis for why their patients’ claims could not be crossed over.
CMS has since learned that concern exists in the provider community concerning whether billing of hardcopy CMS 1500 or UB04 claims or HIPAA version 4010A1 or National Council for Prescription Drug Programs (NCPDP) version 5.1 batch claims will result in Medicare being unable to cross those claims over to COBA supplemental payers that have cut-over to exclusive receipt of crossover claims in the version 5010 837 claim formats or NCPDP D.0 batch claim formats. This is not true.
During the 90-day Version 5010 non-enforcement period (Sunday, January 1, 2012 through Saturday, March 31, 2012), Medicare will have the systematic capability to perform up- or down-version conversion of incoming claim formats (ie. convert incoming hardcopy formats to HIPAA equivalent claim formats and convert incoming version 4010A1 claim formats to 5010 formats and vice-a-versa), in accordance with external supplemental payer specifications concerning production claims format. This practice will discontinue, however, at the conclusion of the 90-day non-enforcement period, with the exception below. (This action is controlled by information that the Common Working File receives concerning individual supplemental payers’ ability to accept HIPAA 5010 or NCPDP D.0 claim formats in “production” mode.)
Note that physicians/practitioners, providers, and suppliers that have authorization under the Administrative Simplification Compliance Act (ASCA) to submit claims using a hardcopy format should know that Medicare has the systematic capability to convert keyed claims into outbound-compliant HIPAA 837 claim formats for crossover claim transmission purposes. This is true at all times, not just during the 90-day non-enforcement period.
What’s Your Plan, Man?
Is your organization preparing for a smooth transition to ICD-10 on Tuesday, October 1, 2013? ICD-10 National Provider Calls, hosted by the CMS Provider Communications Group, can help you prepare for the US healthcare industry’s change from ICD-9 to ICD-10 for diagnosis and inpatient procedure coding.
Video slideshow presentations from the following National Provider Calls are available on the CMS YouTube Channel. These video slideshows include the call slide presentation and audio with captions; each call includes presentations by CMS subject matter experts, followed by a question and answer session.
- ICD-10 Implementation Strategies and Planning – Thursday, November 17, 2011
The ICD-9-CM and ICD-10 Cooperating Parties – CMS, the American Hospital Association (AHA), the American Health Information Management Association (AHIMA), and the Centers for Disease Control and Prevention (CDC) – discuss ICD-10 implementation strategies and planning, and the CMS Provider Billing Group discuss the Medicare FFS claims processing guidance issued in August 2011.
- ICD-10 Implementation Strategies for Physicians – Wednesday, August 3, 2011
CMS subject matter experts discuss how physician offices can prepare for the change to ICD-10 for medical diagnosis and inpatient procedure coding and provide updates on national ICD-10 implementation issues affecting all providers.
- CMS ICD-10 Conversion Activities – Wednesday, May 18, 2011
CMS subject matter experts discuss the ICD-10 conversion process currently taking place within CMS, including a case study from the Coverage and Analysis Group on their transition to ICD-10 for the lab national coverage determinations (NCDs).
Podcasts, complete audio files, and complete written transcripts for these ICD-10 National Provider Calls are also available on the CMS ICD-10 webpage at http://www.CMS.gov/ICD10/
Available 24/7, YouTube video presentations and podcasts make learning about the ICD-10 transition easy and convenient. Check them out today.
Medicare Learning Network Announcements, Updates and Revisions
From the MLN: “Health Professional Shortage Area Bonus Payment Policy Reminders” MLN Matters Article Released – A new MLN Matters® Special Edition Article #SE1202, “Health Professional Shortage Area (HPSA) Bonus Payment Policy Reminders,” has been released in downloadable format. This article is designed to provide education on the HPSA Bonus Payment Program, and provides information about the program and resources that providers can use to determine whether they are eligible to receive the bonus payment.
From the MLN: New “Medicare Coverage of Radiology and Other Diagnostic Services” Fact Sheet Released – A new “Medicare Coverage of Radiology and Other Diagnostic Services” fact sheet (ICN 907164) has been released in downloadable format. This fact sheet is designed to provide education on Medicare coverage and billing information for radiology and other diagnostic services, and includes specific information concerning billing and coding requirements and an overview of coverage guidelines.
From the MLN: New Fast Fact on MLN Provider Compliance Webpage – A new fast fact is now available on the MLN Provider Compliance webpage. This page provides the latest educational products designed to help Medicare Fee-For-Service providers understand – and avoid – common billing errors and other improper activities. Please bookmark this page and check back often as a new fast fact is added each month!
From the MLN: “Acute Care Hospital Inpatient Prospective Payment System” Fact Sheet Revised – The “Acute Care Hospital Inpatient Prospective Payment System” fact sheet (ICN 006815) has been revised and is available in downloadable format. This fact sheet includes information on payment background, the basis for the Acute Care Hospital Inpatient Prospective Payment System payment, payment rates, and how payment rates are set.
From the MLN: “Items and Services That Are Not Covered Under the Medicare Program” Booklet and “Medicare Claim Submission Guidelines” Fact Sheet Now Available in Hardcopy – The “Items and Services That Are Not Covered Under the Medicare Program” booklet (ICN 906765), available now in hardcopy, includes information about the four categories of items and services that are not covered under the Medicare program and applicable exceptions to exclusions and the Advance Beneficiary Notice of Noncoverage.
The “Medicare Claim Submission Guidelines” fact sheet (ICN 906764), available now in hardcopy as well, includes information about applying for a National Provider Identifier and enrolling in the Medicare program, filing Medicare claims, and private contracts with Medicare beneficiaries.
From the MLN: “Medicare Claim Review Programs” Booklet Revised – The revised “Medicare Claim Review Programs: MR, NCCI Edits, MUEs, CERT, and RAC” booklet (ICN 006973) is designed to provide education on the different CMS claim review programs and assist providers in reducing payment errors, including, in particular, coverage and coding errors. It includes frequently asked questions, resources, and an overview of the various programs, including Medical Review, Recovery Audit Contractor, and the Comprehensive Error Rate Testing Program.
From the MLN: “Substance (Other Than Tobacco) Abuse Structured Assessment and Brief Intervention (SBIRT)” Fact Sheet Revised – This revised “Substance (Other Than Tobacco) Abuse Structured Assessment and Brief Intervention (SBIRT)” fact sheet (ICN 904084) is designed to provide education on SBIRT, an early intervention approach that targets those with nondependent substance use to provide effective strategies for intervention prior to the need for more extensive or specialized treatment.
From the MLN: “Non-Specific Procedure Code Description Requirement for HIPAA Version 5010 Claims” MLN Matters Article Released – The new “Non-Specific Procedure Code Description Requirement for HIPAA Version 5010 Claims” MLN Matters Special Edition Article (#SE1138) is designed to provide education on the requirements for non-specific procedure codes for HIPAA 5010 claims, as established in Change Request 7392. It includes guidance to help providers comply with the requirements and submit HIPPA-compliant claims for all non-specific procedure codes.
From the MLN: “Federally Qualified Health Center” Fact Sheet Revised – The revised “Federally Qualified Health Center” fact sheet (ICN 006397) includes the following information: background; FQHC designation; covered FQHC services; FQHC preventive primary services that are not covered; FQHC Prospective Payment System; FQHC payments; and Medicare Prescription Drug, Improvement, and Modernization Act of 2003 provisions that impact FQHCs.
From the MLN: Medicare Preventive Services Series: Part 2, Web-Based-Training Course (WBT) Revised – This WBT is designed to provide education on Medicare Preventive Services. It includes information on Medicare’s coverage for the initial preventive physical exam (IPPE), ultrasound screening for abdominal aortic aneurysm (AAA), screening electrocardiogram (EKG), Annual Wellness Visit (AWV), cardiovascular screening blood tests, diabetes-related services, human immunodeficiency virus (HIV) screening and smoking and tobacco-use cessation counseling services. To access the WBT, visit the MLN Products page, scroll to the “Related Links Inside CMS,” and select the “Web-Based Training (WBT) Courses.”
From the MLN: MLN Guided Pathways (Basic, A, and B) Provider-specific Resource Booklets Revised – The revised MLN Guided Pathways curriculum is designed to allow learners to easily identify and select resources by clicking on topics of interest. The curriculum begins with basic knowledge for all providers and then branches to information for either those enrolling on the 855B, I, and S forms or on the 855A form (or Internet-based PECOS equivalents). The resource booklets are:
- MLN Guided Pathways to Medicare Resources – Basic Curriculum for Health Care Professionals, Suppliers, and Providers
- MLN Guided Pathways to Medicare Resources Intermediate Curriculum for Health Care Providers (Part A)
- MLN Guided Pathways to Medicare Resources Intermediate Curriculum for Health Care Professionals and Suppliers (Part B)
From the MLN: “MLN Guided Pathways Provider-specific” Resource Booklet Revised – The Revised MLN Guided Pathways to Medicare Resources provider-specific resource booklet provides various specialties of healthcare professionals, (physicians, chiropractors, optometrists, podiatrists), nurses (APN, RNCNS, NP, Midwife) PAs, social workers, psychologists, therapists (OT, PT, SLP), dietitians, nutritionists, suppliers (ambulance, ASC, DMEPOS, FQHC, RHC, Labs, mammography, radiation therapy, portable x-ray), and providers (CMHC, CORF, ESRD, HHA, hospice, OPT, pathology and SNF) with resources specific to their specialty including Internet-Only Manuals (IOMs), Medicare Learning Network® publications, CMS webpages, and more. This version includes the addition of pathways for Anesthesiology Assistant/Certified Registered Nurse Anesthetist, Anesthesiologist, Ophthalmologist, and Optometrist, along with a fully developed pathway for Mass Immunization Roster Biller.
All of the MLN Guided Pathways booklets above are available at http://www.CMS.gov/
From the MLN: “Preventive Services Educational Resources for Health Care Professionals” MLN Matters® Article Released – The new “Preventive Services Educational Resources for Health Care Professionals” MLN Matters® Special Edition Article (#SE1142) is designed to provide education on available educational resources related to Medicare-covered preventive services. It includes a list of MLN products that can help Medicare FFS providers understand coverage, coding, reimbursement, and billing requirements related to these services.
From the MLN: “Advanced Payment Accountable Care Organization Model” Fact Sheet Available – The new “Advanced Payment Accountable Care Organization Model” fact sheet (ICN 907403) is designed to provide education on the advance payment model for Accountable Care Organizations (ACOs). It includes a summary of the Advance Payment ACO Model, background, and information on the structure of payments, recoupment of advance payments, eligibility, and the application process.
From the MLN: “Summary of Final Rule Provisions for Accountable Care Organizations Under the Medicare Shared Savings Program” Fact Sheet Available – The new “Summary of Final Rule Provisions for Accountable Care Organizations Under the Medicare Shared Savings Program” fact sheet (ICN 907404) is designed to provide education on the provisions of the final rule that implements the Medicare Shared Savings Program with ACOs. It includes background, information on how ACOs impact beneficiaries, eligibility requirements to form an ACO, and information on monitoring and tying payment to improved care at lower costs.
From the MLN: “Improving Quality of Care for Medicare Patients: Accountable Care Organizations” Fact Sheet Available – The new “Improving Quality of Care for Medicare Patients: Accountable Care Organizations” fact sheet (ICN 907407) is designed to provide education on improving quality of care under ACOs. It includes a table of quality measures under the program.
From the MLN: “Medicare Shared Savings Program and Rural Providers” Fact Sheet Available – The new “Medicare Shared Savings Program and Rural Providers” fact sheet (ICN 907408) is designed to provide education on how the Medicare Shared Savings Program impacts rural providers. It includes information on federally qualified health centers, rural health clinics, critical access hospitals, and how this program impacts them.