If you are a physician, non-physician practitioner or Independent Diagnostic Testing Facility (IDTF) who supplies imaging services and submits claims for the Technical Component (TC) of Advanced Diagnostic Imaging (ADI) procedures to Medicare contractors (carriers and A/B Medicare Administrative Contractors (MACs)), you should know that you must be accredited by Sunday, January 1, 2012. If your facility uses an accredited mobile facility, and you bill for the TC of ADI, you must also be accredited. The accreditation requirement is attached to the biller of the services.
Those not accredited by that deadline will not be able to bill Medicare until they become accredited.
For those planning on seeking accreditation to continue performing the technical component of ADI services, know that accreditation is dependent on the demonstration of quality standards, including (but not limited to):
- Qualifications and responsibilities of medical directors and supervising physicians;
- Qualifications of medical personnel who are not physicians;
- Procedures to ensure that equipment used meets performance specifications;
- Procedures to ensure the safety of beneficiaries;
- Procedures to ensure the safety of person who furnish the imaging; and
- Establishment and maintenance of a quality assurance and quality control program to ensure the reliability, clarity and accuracy of the technical quality of the image.
Additionally, the accreditation process may include:
- Unannounced, random site visits;
- Review of phantom images;
- Review of staff credentialing records and maintenance records;
- Review of beneficiary complaints and patient records;
- Review of quality data and ongoing data monitoring; and
- Triennial surveys.
Frequently Asked Questions
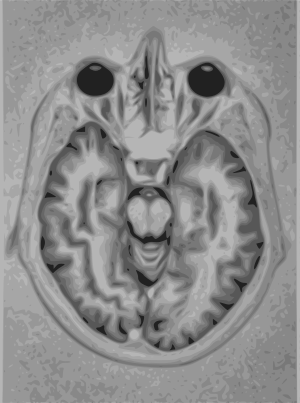
Q: What are ADIs?
A: ADI procedures are defined as MRI, CT and Nuclear Medicine/PET.
Q: As a supplier, what information will I need to transmit to CMS when I become accredited for the TC of advanced imaging?
A: The designated accreditation organization (AO) will transmit the findings of all accreditation decisions to CMS or its contractor when the decision becomes final. The information will include identifying information, the accreditation effective date and those modalities that are included in the accreditation.
Q: What is the process for denying claims after January 1, 2012?
A: Contractors will deny claims with a date of service on or after January 1, 2012, submitted for the TC of the ADI codes with denial code N290 (“Missing/incomplete/invalid rendering provider primary identifier.”) when the provider is not enrolled or accredited by a designated CMS accreditation organization. Contractors shall deny claims with codes submitted with a date of service on or after January 1, 2012, for the TC if the code is not listed on the provider’s eligibility file using claim adjustment reason code (CARC)185 (The rendering provider is not eligible to perform the service billed.)
Q: What happens if I am already accredited and will be up for re-accreditation in 2012?
A: In the case of a supplier that is accredited before January 1, 2010 by one of the designated accreditation organizations, the supplier is considered to have been accredited by an organization for the period such accreditation is in effect. The supplier would have had to remain in good standing and have an active accreditation on 1/1/2012 and must apply for reaccreditation within the time frame specified by the accreditation organization.
Q: Do hospitals have to receive imaging accreditation for the Technical Component (TC) of advanced imaging that is performed under the prospective payment system?
A: Hospitals are generally exempt from this requirement. In Section 1834(e) of the Social Security Act and codified in §414.68(a), it is stated that the imaging accreditation requirement applies only to suppliers of the TC of advanced diagnostic imaging services for which payment is made under the physician fee schedule. Since hospitals generally are not paid pursuant to such schedule, this accreditation rule is inapplicable. Thus, providers will list ADI equipment and CPT code information in their initial and updated enrollment applications. Accreditation status will be provided to the Medicare Administrative Contractors by the ACO’s.
Q: Do the accreditation requirements apply to the radiologists that interpret the images?
A: The accreditation will apply only to the suppliers producing the images themselves, and not to the physician’s interpretation of the image. However, all interpreting physicians must meet the accreditation organizations published standards for qualifications and responsibilities of medical directors and supervising physicians, such as training in advanced diagnostic imaging services in a residency program and expertise obtained through experience or continuing medical education. Oral surgeons and dentists must be accredited if they perform the Technical Component of MRI, CT or Nuclear Medicine for the technical component of the codes that require ADI accreditation.
Q: Is Fluoroscopy covered under the new accreditation requirement?
A: MIPPA (Section 135 (a) of the Medicare Improvements for Patients and Providers Act of 2008) expressly excludes from the accreditation requirement x-ray, ultrasound, screening and diagnostic mammography and fluoroscopy procedures. The law also excludes from the CMS accreditation requirement diagnostic and screening mammography which are subject to quality oversight by the Food and Drug Administration under the Mammography Quality Standards Act.
Q: How do I choose which AO to accredit my organization?
A: As a supplier, you will need to contact each of the three designated organizations to determine which accrediting organization meets your specific business model and philosophy for patient care. Some of the factors affecting your decision should be review of the quality standards, accreditation cycle, accreditation processes and price.
Q: Who are the accreditation organizations recognized by CMS to comply with the MIPPA accreditation requirement?
A: The Centers for Medicare & Medicaid Services (CMS) approved three national accreditation organizations – the American College of Radiology, the Intersocietal Accreditation Commission, and The Joint Commission – to provide accreditation services for suppliers of the TC of advanced diagnostic imaging procedures.
Q: What does it cost to be accredited?
A: The accreditation costs vary by accreditation organization. The average cost for one location and one modality is approximately $3,500 every 3 years.
Q: How do I contact the accreditation organizations (AOs)?
A: Call or e-mail each of the accreditation organizations to determine the one
that best fits your business needs. The accreditation organizations each have
their own published standards. Follow all of the application requirements so that your application is not delayed. It may take up to 5 months to be accredited. So, you really must start now to be sure to meet the January 1, 2012, date.To obtain additional information about the accreditation process, please contact the accreditation organizations shown below.
American College of Radiology (ACR)
1891 Preston White Drive
Reston, VA 20191-4326
1-800-770-0145
—
Intersocietal Accreditation Commission (IAC)
6021 University Boulevard, Suite 500
Ellicott City, MD 21043
1-800-838-2110
—
The Joint Commission (TJC)
Ambulatory Care Accreditation Program
One Renaissance Boulevard
One Renaissance, IL 60181
1-630-792-5286
For more information about the enrollment procedures, see the Medicare Learning Network® (MLN) article MM7177, “Advanced Diagnostic Imaging Accreditation Enrollment Procedures,” available here.
If you are a physician or non-physician practitioner supplying the Technical
Component of ADI, see the MLN article MM7176, “Accreditation for Physicians and Non-Physician Practitioners Supplying the Technical Component (TC) of Advanced Diagnostic Imaging (ADI) Service,” available here.