Medicare Signature Requirements
The purpose of a rendering/treating/ordering practitioner’s signature in patients’ medical records, operative reports, orders, test findings, etc., is to demonstrate the services have been accurately and fully documented, reviewed and authenticated. It confirms the provider has certified the medical necessity and reasonableness for the service(s) submitted to the Medicare program for payment consideration. For medical review purposes, Medicare requires that services provided/ordered be authenticated by the author.
Let’s define some terms first.
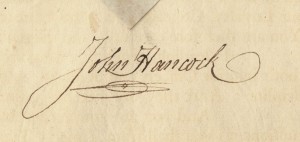
Handwritten Signature – a handwritten signature is a mark or sign by an individual on a document to signify knowledge, approval, acceptance or obligation and of the document.
Digitized Signature – a digitized signature is an electronic image of an individual’s handwritten signature reproduced in its identical form using a pen tablet.
Signature Log – A signature log is a typed listing of the provider(s) identifying their name with a corresponding handwritten signature. This may be an individual log or a group log. A signature log may be used to establish signature identity as needed throughout the medical record documentation. On behalf of a health care provider, the practice manager may create a signature log at any time, and Medicare Contractors will accept all submitted signature logs regardless of the date on which they were created.
Signature Attestation – A signature attestation is a statement that must be signed and dated by the author of the medical record entry and must contain sufficient information to identify the beneficiary. SAMPLE verbiage:
I, _____[print full name of the physician/practitioner]___, hereby attest that the
medical record entry for _____[date of service]___ accurately reflects signatures/notations that I made in my capacity as _____[insert provider credentials, e.g., M.D.]___ when I treated/diagnosed the above listed Medicare beneficiary. I do hereby attest that this information is true, accurate and complete to the best of my knowledge and I understand that any falsification, omission, or concealment of material fact may subject me to administrative, civil, or criminal liability.
Electronic Signature – Electronic signatures usually contain date and timestamps and include printed statements, e.g., “electronically signed by,” or “verified/reviewed by,” followed by the practitioner’s name and preferably a professional designation. Note: The responsibility and authorship related to the signature should be clearly defined in the record. Example of an acceptable electronic signature: “Electronically Signed By: John Doe, M.D. 08/01/2008 @ 06:26 A “
Digital Signature – a digital signature differs from an electronic signature in that it is an electronic method of a written signature that is typically generated by special encrypted software that allows for sole usage.
NOTE: Be aware that electronic and digital signatures are not the same as “auto-authentication” or “auto-signature” systems, some of which do not mandate or permit the provider to review an entry before signing. Indications that a document has been “signed but not read” are not acceptable as part of the medical record.
Signature stamp – a signature stamp is a likeness of a handwritten signature used by administrative staff on medical records. Signature stamps on medical records are NO longer recognized as valid authentication for Medicare signature purposes and may result in payment denials by Medicare.
Rules Medicare Auditors Use for Signatures
- If the signature is illegible or missing from the medical documentation (other than an order), the review contractor shall consider evidence in a signature log or attestation statement to determine the identity of the author of a medical record entry.
- If the signature is missing from an order, the review contractor shall disregard the order during the review of the claim (i.e., the reviewer will proceed as if the order was not received). Signature attestations are not allowable for orders.
- For a signature to be valid, the following criteria must be met:
- Services that are provided or ordered must be authenticated by the ordering practitioner.
- Signatures are handwritten or electronic. Stamped signatures are not acceptable.
- Signatures are legible.
- Medicare does not accept retroactive orders. If the practitioner’s signature is missing from the medical record, the practice should submit an attestation statement from the author of the medical record.
- Your contractor may offer specific guidance regarding addenda to medical records. If the order is unsigned, you may submit progress notes showing intent to order the tests. The progress notes must specify what tests you ordered. A note stating “Ordering Lab” is not sufficient. If the orders and the progress notes are unsigned, your facility or practice will be assessed an error, which may involve recoupment of an overpayment.
- You may submit a signature log or attestation statement to support the identity of the illegible signature. If the original record contains a printed signature below the illegible signature, this may be accepted.
- Documentation must contain enough information to determine the date on which the service was performed or ordered. If the entry immediately above or below the entry is dated, medical review may reasonably assume the date of the entry in question.
- Reports or any records that are dictated and/or transcribed, but do not include valid signatures “finalizing and approving” the documents are not acceptable for reimbursement purposes. Corresponding claims for these services will be denied.
- Acceptable signature phrasing is
- ‘Electronically signed by’ with provider’s name
- ‘Verified by’ with provider’s name ‘Reviewed by’ with provider’s name
- ‘Released by’ with provider’s name
- ‘Signed by’ with provider’s name
- ‘Signed before import by’ with provider’s name
- ‘Signed: John Smith, M.D.’ with provider’s name
- Digitalized signature: Handwritten and scanned into the compute.
- ‘This is an electronically verified report by John Smith, M.D.’
- ‘Authenticated by John Smith, M.D.’
- ‘Authorized by: John Smith, M.D.’
- ‘Digital Signature: John Smith, M.D.’
- ‘Confirmed by’ with provider’s name
- ‘Closed by’ with provider’s name
- ‘Finalized by’ with provider’s name
- ‘Electronically approved by’ with provider’s name
Unique Signature Situations
Incident-to Services – a physician’s professional services means that the services or supplies are furnished as an integral, although incidental, part of the physician’s personal professional services in the course of diagnosis or treatment of an injury or illness. Only the Past, Family, and Social History (PFSH) and Review of Systems (ROS) may be documented by ancillary personnel incident to and incorporated in to the E/M documentation, which must be reviewed and signed by the billing provider.
Services of non-physician practitioners (NPPs) – ordinarily performed by the physician such as minor surgery, setting casts or simple fractures, reading x-rays, and other activities that involve evaluation or treatment of a patient’s condition are also covered as services incident to a physician’s professional services. If the NPP performs an entire service incident-to the physician (office/clinic/home settings only), the medical record may be signed by the NPP or the physician.
Split/shared services –
- Office setting: When an E/M service in an office setting is a shared/split encounter between a physician and a non-physician practitioner (NP, PA, CNS or CNM), the service is considered to have been performed “incident to” if the requirements for “incident to” are met and the patient is an established patient. The service is reported using the physician’s billing number. The physician must sign.If “incident to” requirements are not met for the shared/split E/M service, the service must be billed under the NPP’s billing number, and payment will be made at the appropriate physician fee schedule payment. The billing NPP provider must sign.Hospital-based setting: When a hospital inpatient/hospital outpatient or emergency department E/M is shared between a physician and an NPP from the same group practice and the physician provides any face-to-face portion of the E/M encounter with the patient, the service may be billed under either the physician’s or the NPP’s number. However, if there was no face-to-face encounter between the patient and the physician (e.g., even if the physician participated in the service by only reviewing the patient’s medical record) then the service may only be billed under the NPP’s number. Payment will be made at the appropriate physician fee schedule rate based on the billing number entered on the claim. The billing provider (physician or NPP) as determined above must sign.
Assistant at surgery – It is not required that a surgical assistant also sign the operative report in addition to the responsible surgeon when reference is made in the note that identifies the assistant, provided that the report contains an acceptable signature by the responsible surgeon
Physician was present at the visit, but was unable to sign the record due to death or relocation – If the provider is in a group practice, another provider within the group may sign on his/her behalf; however the following information must be provided:
The submitting provider, John W. Smith, M.D., is unable to sign this medical record because he expired on 10/08/08.
or
John W. Smith, M.D. relocated to Colorado on 10/08/08 and was unable to sign this medical record.
Dictated Notes and Use of Initials
The physician must review the transcribed note to correct any errors and affirm the note’s contents for it to be considered the final documentation of the service.
- It is not sufficient that the provider is designated as dictating the note or his/her name is present in the record.
- If an illegible handwritten signature is present and the record contains no other identification of the author (i.e., printed name below, or letterhead with name) a signature log or attestation statement must be included with a response to the auditor documentation request.
- If the record is missing a signature, an attestation statement must be included in the response to the auditor’s documentation request.
- A legible signature that includes the provider’s full name and credentials is always the best practice.
- Initials are acceptable if signed over a typed or printed name.
- Without a typed name to identify the author, a signature log or attestation statement must be submitted or services may be denied.